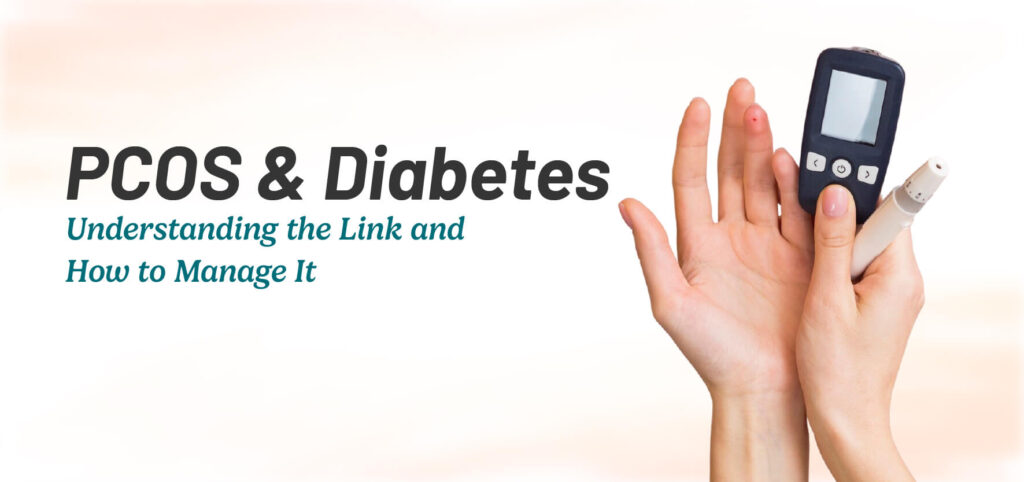
Discover the symptoms, root causes, and science-backed treatments for PCOS and insulin resistance. Learn when to seek help and how to manage it effectively.
Overview
The intricate dance of hormones within the female body, when disrupted, can lead to a condition known as Polycystic Ovary Syndrome (PCOS), often accompanied by its metabolic counterpart, insulin resistance. This intricate relationship impacts a substantial portion of women, creating a ripple effect that extends beyond menstrual irregularities to affect overall metabolic health. It’s not merely about missed periods or weight fluctuations; it’s a systemic condition that can influence energy levels, skin integrity, emotional well-being, and long-term health. Understanding the nuanced interplay between PCOS and insulin resistance is paramount for effective management and empowering individuals to regain control over their health.
This condition demands attention, as its effects can significantly diminish quality of life if left unaddressed. Recognizing the subtle cues and seeking timely intervention can profoundly alter the trajectory of this condition, enabling individuals to navigate their health with greater confidence and resilience.
Symptoms of PCOS and Insulin Resistance
- Irregular or absent menstrual cycles, characterized by unpredictable timing, prolonged intervals, or complete cessation of periods. This disruption reflects underlying hormonal imbalances.
- Noticeable and persistent weight gain, particularly around the abdominal region, which can be resistant to traditional weight loss strategies. This is often a sign of underlying insulin resistance.
- Hirsutism, the excessive growth of dark, coarse hair in areas typically associated with male hair patterns, such as the face, chest, and back. This symptom arises from elevated androgen levels.
- Skin issues, including persistent acne, oily skin, and dark patches (acanthosis nigricans), reflecting hormonal fluctuations and insulin resistance.
- Persistent fatigue and low energy levels, even after adequate rest, stemming from hormonal imbalances and metabolic dysregulation.
- Acanthosis nigricans, the development of dark, velvety patches of skin in folds and creases, indicating heightened insulin levels.
- Hair thinning or male-pattern baldness, reflecting the influence of excess androgens.
- Mood fluctuations, including increased irritability, anxiety, and depressive tendencies, are linked to hormonal shifts and the chronic nature of the condition.
- Disrupted sleep patterns, including insomnia and sleep apnea, which can further exacerbate metabolic issues.
- Pelvic pain, which can be chronic or intermittent, and is often related to the presence of ovarian cysts.
When to See a Doctor
If you observe a cluster of these symptoms, especially if they include marked changes in your menstrual cycle, unexplained weight gain, or the development of hirsutism, seeking professional medical advice is essential. Early detection and intervention can significantly improve long-term health outcomes and prevent the development of serious complications. Immediate consultation is necessary if you experience severe abdominal discomfort, abnormal vaginal bleeding, or sudden, significant changes in your health. Delaying diagnosis can lead to worsening insulin resistance, increased risk of related health problems, and a diminished quality of life.
Causes of PCOS and Insulin Resistance
Biological Causes The root causes of PCOS and insulin resistance involve a complex interplay of internal factors. Genetic predispositions play a significant role, with a tendency for the condition to cluster within families. Hormonal imbalances, particularly an increase in androgens, such as testosterone, are central to the condition. Insulin resistance, where the body’s cells do not respond effectively to insulin, triggers a cascade of hormonal events, leading to elevated insulin levels. This creates a feedback loop, exacerbating both the hormonal disruptions and the metabolic challenges. The ovaries, influenced by these hormonal imbalances, produce multiple small follicles, contributing to the characteristic polycystic appearance. The interplay between genetics, hormones, and metabolism creates a complex condition that requires a multifaceted approach to management.

Lifestyle Triggers
Daily habits significantly influence the development and severity of PCOS and insulin resistance. A diet heavy in processed foods, refined carbohydrates, and sugars can contribute to insulin spikes and resistance, worsening the metabolic aspects of the condition. A lack of regular physical activity can further impair insulin sensitivity, exacerbating metabolic dysfunction. Chronic stress can also play a role, as elevated stress hormones, such as cortisol, can disrupt the delicate hormonal balance, contributing to insulin resistance and hormonal imbalances. These lifestyle factors, when combined, create a fertile ground for the development and progression of PCOS and insulin resistance.
Risk Factors
Several factors heighten the risk of developing PCOS and insulin resistance. A family history of either condition increases susceptibility, indicating a genetic predisposition. Excess weight, particularly abdominal fat, is a significant risk factor, as it contributes to insulin resistance and hormonal imbalances. A sedentary lifestyle, characterized by low physical activity levels, further exacerbates the risk of metabolic dysfunction. Certain genetic backgrounds and ethnicities may also predispose individuals to these conditions.
Complications
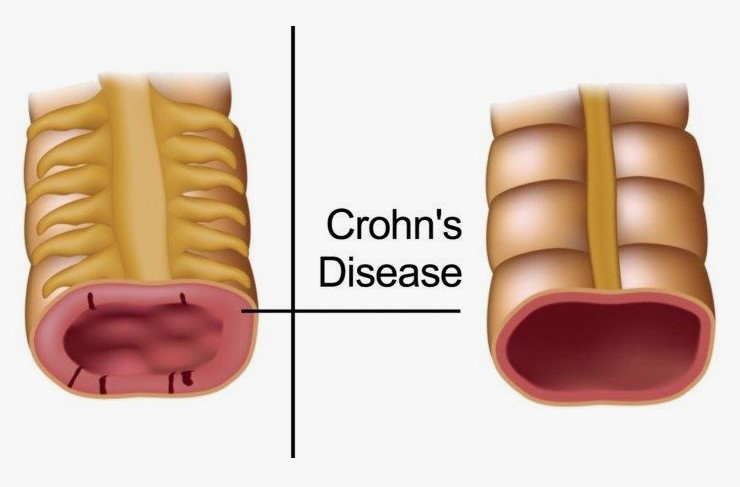
If left unaddressed, PCOS and insulin resistance can lead to a range of serious health complications, impacting long-term well-being. These include an increased risk of type 2 diabetes, characterized by chronic hyperglycemia, and cardiovascular problems, such as heart disease and stroke, due to metabolic abnormalities. Endometrial abnormalities, including hyperplasia and cancer, are also associated with prolonged unopposed estrogen exposure. Fertility challenges are common, as hormonal imbalances disrupt ovulation, making conception difficult. Additionally, mental health can be significantly affected, with increased rates of anxiety, depression, and other mood disorders. Sleep apnea, non-alcoholic fatty liver disease, and other metabolic issues are also common.
Diagnosis
- Blood tests to assess hormone levels, including androgens (testosterone, DHEAS), estrogen, progesterone, and luteinizing hormone (LH). These tests help evaluate hormonal imbalances and identify specific patterns associated with PCOS.
- Pelvic ultrasound to visualize the ovaries and assess for the presence of multiple small follicles (cysts), a characteristic feature of PCOS. This imaging technique provides valuable information about ovarian morphology.
- Glucose tolerance tests to evaluate insulin response and glucose metabolism. These tests, such as the oral glucose tolerance test (OGTT), help diagnose insulin resistance and impaired glucose tolerance.
- Lipid profile to assess cholesterol and triglyceride levels, which can be affected by insulin resistance. This helps evaluate cardiovascular risk.
- Fasting insulin level assessment. This will help to determine the level of insulin the body produces when fasting. This is a crucial test to determine the level of insulin resistance.
Treatment Options
- Medications to improve insulin sensitivity and regulate menstrual cycles, such as metformin. These medications help address the metabolic aspects of PCOS.
- Hormonal therapies, including birth control pills, to manage androgen levels and related symptoms, such as acne and hirsutism. These therapies help regulate menstrual cycles and improve hormonal balance.
- Dietary modifications to improve insulin sensitivity and promote weight management. A balanced diet focused on low glycemic index foods, such as whole grains, fruits, vegetables, and lean proteins, is crucial.
- Regular physical activity to enhance metabolic health and improve hormonal balance. A combination of cardiovascular exercise and strength training is recommended.
- Inositol supplements, which have shown promise in improving insulin sensitivity and regulating menstrual cycles in women with PCOS. These supplements can be a valuable adjunct to conventional treatment.
- Anti-androgen medications, such as spironolactone, which can help manage hirsutism and acne by blocking the effects of androgens.
- Fertility treatments, such as clomiphene citrate or letrozole, for women with PCOS who are trying to conceive. These treatments help induce ovulation.
- Bariatric surgery, in cases of severe obesity, can significantly improve insulin sensitivity and PCOS symptoms. This option is considered when other treatments are ineffective.
Learn more about natural remedies for PCOS and Insulin Resistance here: /natural-remedies-for-pcos-and-insulin-resistance.





[…] Understanding PCOS and Insulin Resistance: Symptoms, Causes, and Proven Solutions […]