Discover the symptoms, root causes, and science-backed treatments for Crohn’s Disease. Learn when to seek help and how to manage it effectively.
Overview of Disease
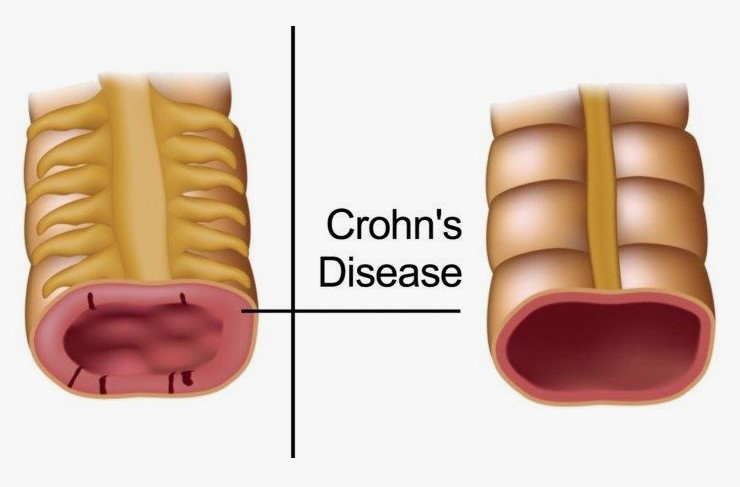
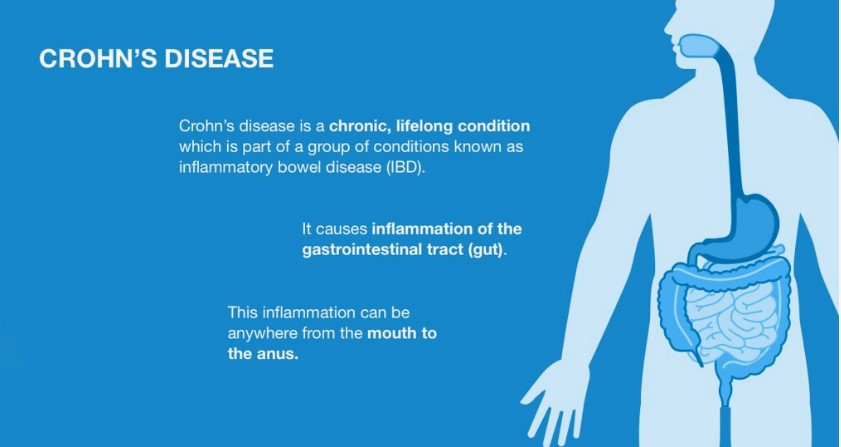
Have you been experiencing a persistent and unsettling discomfort in your abdomen, a relentless cycle of bowel disturbances, or an overwhelming sense of fatigue that seems to have no discernible cause? These could be signals from your body, early indicators of a complex and chronic condition known as Crohn’s Disease. Crohn’s Disease falls under the umbrella of inflammatory bowel diseases (IBD), a group of disorders characterized by chronic inflammation of the digestive tract. Unlike its close relative, ulcerative colitis, which primarily affects the colon, Crohn’s Disease can cast its inflammatory shadow across any segment of the gastrointestinal (GI) tract, from the oral cavity down to the anus. This means that the location and severity of inflammation can vary significantly from one individual to another, leading to a diverse range of symptoms and challenges.
Symptoms of Crohn’s Disease
The clinical presentation of Crohn’s Disease is highly variable, influenced by the location and extent of inflammation within the digestive tract, as well as the severity and duration of the disease. Symptoms can range from mild and intermittent to severe and persistent, often characterized by periods of active disease (flare-ups) followed by periods of reduced symptoms (remission). Recognizing the diverse range of potential symptoms is crucial for both individuals and healthcare professionals to facilitate timely diagnosis and appropriate management. Some of the key and frequently reported symptoms of Crohn’s Disease include:
- Persistent diarrhea: This is often one of the most common symptoms experienced by individuals with Crohn’s. The inflammation in the bowel can disrupt the normal absorption of fluids and electrolytes, leading to frequent, loose, and sometimes urgent bowel movements. Diarrhea may be accompanied by abdominal cramping and pain.
- Abdominal pain and cramping: Pain in the abdomen is another hallmark symptom of Crohn’s Disease. The inflammation and irritation of the bowel wall can cause significant discomfort, ranging from mild, intermittent cramping to severe, persistent pain. The location of the pain can vary depending on the part of the digestive tract that is most affected.
- Unexplained weight loss: Chronic inflammation can interfere with the body’s ability to absorb nutrients properly, leading to unintentional and significant weight loss. Additionally, the discomfort and other symptoms associated with Crohn’s Disease can reduce appetite and oral intake, further contributing to weight loss.
Beyond these primary symptoms, individuals with Crohn’s Disease may also experience a range of other manifestations, including:
- Urgent need to have bowel movements.
- Feeling that the bowels are not completely emptied after a bowel movement.
- Nausea and vomiting.
- Loss of appetite.
- Fever.
- Night sweats.
- Skin problems, such as rashes or nodules.
- Eye inflammation (uveitis, iritis).
- Joint pain and inflammation (arthritis).
- Mouth ulcers.
- Anal fissures (small tears in the lining of the anus).
- Perianal disease, including fistulas and abscesses around the anus.
It is important to emphasize that the specific symptoms and their severity can vary greatly among individuals with Crohn’s Disease. Some individuals may experience predominantly bowel-related symptoms, while others may have more prominent extraintestinal manifestations (symptoms affecting other parts of the body). The unpredictable nature of Crohn’s Disease, with its cycles of flare-ups and remissions, further contributes to the variability of symptom presentation over time.
When to See a Doctor
Recognizing the potential signs and symptoms of Crohn’s Disease and seeking timely medical attention is crucial for accurate diagnosis, prompt initiation of treatment, and ultimately, better long-term management of the condition. Ignoring persistent or concerning symptoms can lead to delays in diagnosis, allowing the inflammation to progress and potentially increasing the risk of developing serious complications. It is imperative to consult a healthcare professional if you experience any of the following persistent or troublesome symptoms:
- Persistent diarrhea that lasts for more than a few weeks, especially if it is frequent, watery, or accompanied by abdominal pain.
- Recurrent or severe abdominal pain and cramping that interferes with daily activities.
- Unexplained and unintentional weight loss.
- Noticeable blood in your stool.
- Persistent fatigue that is not relieved by rest.
- Fever that occurs without an obvious infection.
- Development of skin rashes, eye pain, or joint pain, especially in conjunction with gastrointestinal symptoms.
Early diagnosis by a qualified healthcare professional, typically a gastroenterologist (a doctor specializing in digestive system disorders), is essential for several reasons. Firstly, it allows for the differentiation of Crohn’s Disease from other conditions that may present with similar symptoms, such as irritable bowel syndrome (IBS), ulcerative colitis, or infections. Secondly, early intervention with appropriate treatment strategies can help to control inflammation, alleviate symptoms, prevent disease progression, and reduce the risk of developing complications. Thirdly, a timely diagnosis enables individuals with Crohn’s Disease to receive the necessary education, support, and resources to effectively manage their condition and improve their overall quality of life.
Causes of Crohn’s Disease
The precise etiology of Crohn’s Disease remains an area of active research, and currently, there is no single, definitive cause that has been identified. However, the prevailing scientific understanding is that Crohn’s Disease arises from a complex interplay of several contributing factors, including genetic predisposition, a dysregulated immune response, and environmental triggers. These factors likely interact in a multifaceted manner to initiate and perpetuate the chronic inflammation that characterizes Crohn’s Disease. The primary contributing factors can be broadly categorized into biological causes and environmental triggers.
Biological Causes
The biological underpinnings of Crohn’s Disease are thought to involve a combination of an abnormal immune response to the gut microbiota in genetically susceptible individuals:
- Dysregulated Immune Response: The cornerstone of Crohn’s Disease pathogenesis is an aberrant immune response within the gastrointestinal tract. In healthy individuals, the immune system coexists peacefully with the trillions of bacteria, viruses, and fungi that reside in the gut (the gut microbiota). However, in Crohn’s Disease, the immune system appears to mistakenly identify certain components of the gut microbiota as foreign and harmful. This misidentification triggers an inappropriate and sustained autoimmune response, leading to chronic inflammation of the bowel wall. The exact triggers that initiate this abnormal immune response are still being investigated, but it is believed to involve a complex interplay of immune cells, signaling molecules (cytokines), and the intestinal lining.
- Genetic Predisposition: While Crohn’s Disease is not solely a genetic disorder, there is a strong genetic component to its susceptibility. Individuals with a family history of IBD, particularly Crohn’s Disease, have a significantly higher risk of developing the condition. Numerous genes have been identified that are associated with an increased risk of Crohn’s Disease. These genes often play roles in immune system function, the integrity of the gut barrier, and the body’s response to microbes. Research from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) has highlighted the role of NOD2, a gene involved in the immune system’s recognition of bacterial components, as one of the first and most well-studied susceptibility genes for Crohn’s Disease. However, it is important to note that having these genes does not guarantee the development of Crohn’s Disease; rather, they increase an individual’s susceptibility when combined with other factors.
Environmental Triggers
While biological factors create a foundation of susceptibility, various environmental factors are thought to play a significant role in triggering the onset or exacerbating the course of Crohn’s Disease:
- Smoking: Cigarette smoking is one of the most well-established environmental risk factors for Crohn’s Disease. Studies have consistently shown that smokers are at a higher risk of developing Crohn’s Disease compared to non-smokers. Furthermore, smoking is associated with more severe disease, a greater likelihood of needing surgery, and a reduced response to certain medications. The exact mechanisms by which smoking influences Crohn’s Disease are not fully understood but may involve alterations in the gut microbiota, impaired immune regulation, and increased intestinal permeability.
- Gut Microbiota: The trillions of microorganisms that reside in the human gut play a crucial role in digestion, nutrient absorption, and immune system development. Alterations in the composition and function of the gut microbiota (dysbiosis) are increasingly recognized as a potential contributing factor to Crohn’s Disease. It is hypothesized that in genetically susceptible individuals, an imbalance in the gut microbiota may trigger or perpetuate the abnormal immune response that characterizes Crohn’s Disease. Research is ongoing to understand the specific microbial species and their interactions with the host immune system in the context of Crohn’s Disease.
- Infections: While Crohn’s Disease is not caused by a specific infection, some researchers hypothesize that certain infections early in life or chronic low-grade infections may play a role in triggering the disease in genetically susceptible individuals. However, a definitive infectious agent has not been identified.
- Diet: The role of diet in the development and management of Crohn’s Disease is complex and still being investigated. While diet is not considered a primary cause, certain dietary patterns, such as high intake of processed foods and low intake of fruits and vegetables, may influence the gut microbiota and potentially contribute to inflammation in some individuals. Specific dietary components may also trigger symptoms in some people with established Crohn’s Disease.
- Stress: While stress is not believed to be a direct cause of Crohn’s Disease, it can exacerbate symptoms and trigger flare-ups in some individuals. The complex interplay between the brain and the gut (the gut-brain axis) is increasingly recognized, and stress can influence gut motility, inflammation, and immune function.
Risk Factors
Identifying risk factors for Crohn’s Disease can help individuals and healthcare professionals understand who may be at increased susceptibility to developing the condition. While some risk factors are not modifiable, awareness of these factors can prompt earlier vigilance for symptoms and facilitate timely medical evaluation if they arise. The key risk factors associated with an increased likelihood of developing Crohn’s Disease include:
- Family History: As mentioned previously, having a first-degree relative (parent, sibling, or child) with Crohn’s Disease significantly increases an individual’s risk. This strong familial association underscores the important role of genetic factors in susceptibility to the disease. The risk is even higher if multiple family members are affected.
- Age: Crohn’s Disease can be diagnosed at any age, but it is most commonly diagnosed in adolescents and young adults, typically between the ages of 20 and 30. However, a significant number of individuals are also diagnosed later in life.
- Smoking: Cigarette smoking is a well-established and modifiable risk factor for Crohn’s Disease. Smokers are not only more likely to develop the disease but also tend to have more severe disease, a greater risk of complications, and a poorer response to treatment compared to non-smokers. Quitting smoking is strongly recommended for individuals with or at risk of Crohn’s Disease.
It is important to remember that having one or more of these risk factors does not mean that an individual will definitely develop Crohn’s Disease. Many people with risk factors never develop the condition, while others with no known risk factors do. Understanding these risk factors can, however, increase awareness and prompt individuals to seek medical attention if they experience symptoms suggestive of Crohn’s Disease.
Complications of Disease
Chronic inflammation associated with Crohn’s Disease can lead to a variety of serious and potentially life-altering complications affecting the digestive tract and other parts of the body. The development and severity of these complications often depend on the duration and extent of the disease, as well as the effectiveness of treatment. Recognizing these potential complications is crucial for proactive management and timely intervention to minimize their impact on an individual’s health and quality of life. Some of the major long-term complications of Crohn’s Disease include:
- Strictures: Chronic inflammation can lead to scarring and thickening of the bowel wall, resulting in narrowing of the intestinal passage, known as strictures. These strictures can obstruct the flow of stool, causing abdominal pain, bloating, vomiting, and potentially requiring surgical intervention to dilate or remove the narrowed segment.
- Fistulas: These are abnormal connections or tunnels that can form between different parts of the digestive tract (e.g., between the small intestine and the colon), between the digestive tract and other organs (e.g., the bladder or vagina), or between the digestive tract and the skin (perianal fistulas around the anus). Fistulas can cause pain, infection, and drainage and often require medical or surgical treatment.
- Abscesses: Collections of pus can form in the abdominal area due to inflammation and infection in the bowel wall. Abscesses can cause fever, pain, and tenderness and often require drainage, either through imaging-guided procedures or surgery, along with antibiotic treatment.
- Malnutrition and Anemia: Chronic inflammation and damage to the intestinal lining can impair the absorption of essential nutrients, leading to malnutrition. This can result in weight loss, fatigue, and vitamin and mineral deficiencies. Anemia (low red blood cell count) is also common in Crohn’s Disease, often due to chronic blood loss from the inflamed bowel or deficiencies in iron or vitamin B12.
- Anal Fissures: These are small tears in the lining of the anus that can cause pain, bleeding, and discomfort during bowel movements. They are more common in individuals with Crohn’s Disease due to chronic inflammation in the perianal area.
- Perianal Disease: This encompasses a range of problems affecting the area around the anus, including fistulas, abscesses, and skin tags. Perianal disease can be particularly challenging to manage and can significantly impact quality of life.
- Increased Risk of Colon Cancer: Individuals with Crohn’s Disease affecting the colon (Crohn’s colitis) have an increased risk of developing colorectal cancer, particularly if the disease has been present for many years and involves a significant portion of the colon. Regular colonoscopic surveillance with biopsies is recommended for these individuals to screen for precancerous changes.
- Extraintestinal Manifestations: Crohn’s Disease is not limited to the digestive tract and can affect other parts of the body. These extraintestinal manifestations can include:
- Joint problems (arthritis): Inflammation of the large joints (peripheral arthritis) or the spine (ankylosing spondylitis).
- Skin problems: Rashes, such as erythema nodosum or pyoderma gangrenosum.
- Eye inflammation: Uveitis or iritis, causing pain and vision problems.
- Liver and bile duct problems: Primary sclerosing cholangitis (PSC).
- Kidney stones.
The risk of developing these complications underscores the importance of effective long-term management of Crohn’s Disease aimed at controlling inflammation, preventing flare-ups, and maintaining remission. Regular medical follow-up, adherence to prescribed medications, and lifestyle modifications play a crucial role in minimizing the likelihood and severity of these potential complications. Read More>>>