Discover the symptoms, root causes, and science-backed treatments for Epilepsy. Learn when to seek help and how to manage it effectively.
Epilepsy Overview
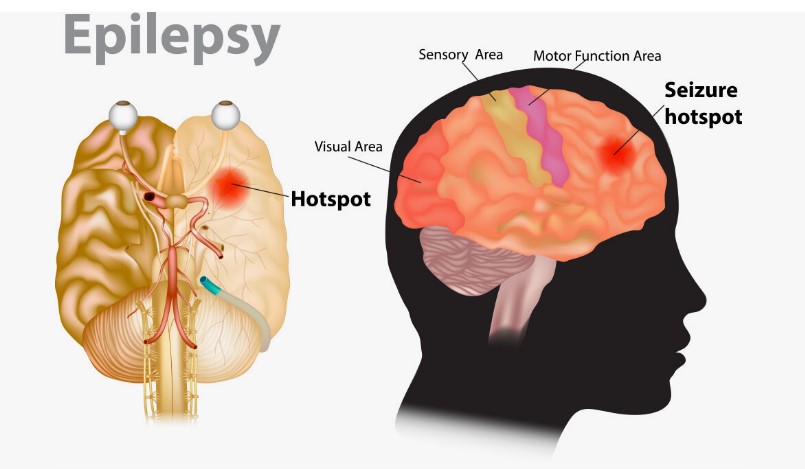
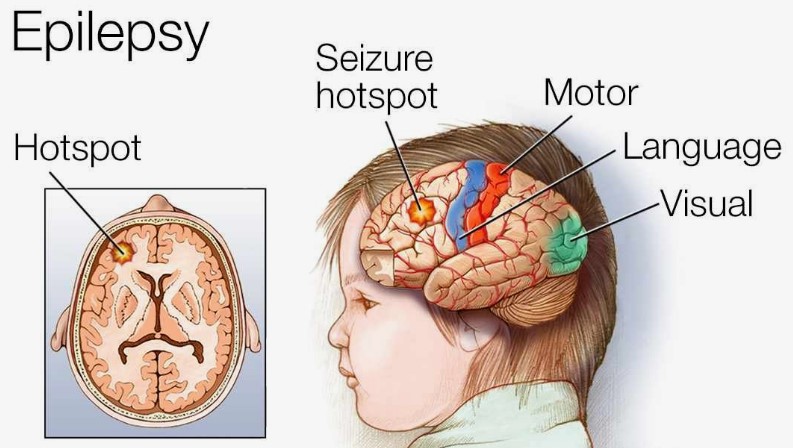
Have you or someone you know experienced the sudden and unpredictable disruption of normal consciousness or motor control that characterizes a seizure? Epilepsy is a chronic neurological disorder defined by the occurrence of recurrent, unprovoked seizures. These seizures are transient events resulting from abnormal, excessive, or synchronous neuronal activity in the brain.
The global impact of Epilepsy is substantial. According to the World Health Organization (WHO), approximately 50 million individuals worldwide live with this condition, making it one of the most prevalent neurological disorders, affecting people of all ages, races, and socioeconomic backgrounds.
Symptoms of Epilepsy
The hallmark of Epilepsy is the occurrence of seizures, but the clinical presentation of these events can vary dramatically depending on the area of the brain involved and the extent of the abnormal electrical activity. It is essential to recognize the wide spectrum of seizure types and their associated symptoms:
- Uncontrolled jerking movements (convulsions): These are perhaps the most widely recognized symptom of a seizure, often associated with what is known as a tonic-clonic seizure (formerly grand mal). This type involves a loss of consciousness, stiffening of the body (tonic phase), followed by rhythmic jerking movements of the limbs (clonic phase). However, not all seizures involve convulsions.
- Loss of consciousness: Some seizures, including tonic-clonic and some focal seizures, can involve a complete loss of consciousness, often followed by a period of postictal confusion or drowsiness.
- Sensory disturbances (e.g., tingling, visual changes): Focal seizures (formerly partial) can originate in specific areas of the brain responsible for sensory processing.
Beyond these primary symptoms, individuals experiencing a seizure may also exhibit:
- Sudden falls without apparent cause.
- Muscle stiffness or sudden loss of muscle tone (atonic seizures).
- Brief muscle jerks (myoclonic seizures).
- Changes in emotions or sensations (e.g., sudden feelings of fear, déjà vu).
- Bowel or bladder control issues during a seizure.
It is crucial to remember that the symptoms experienced during a seizure are transient. However, the unpredictable nature of seizures and the potential for injury or other complications underscore the importance of effective management. Recognizing the diverse manifestations of seizures is the first step towards seeking appropriate medical attention and obtaining an accurate diagnosis.
When to See a Doctor
Prompt medical evaluation is paramount in cases of suspected Epilepsy. The circumstances surrounding a seizure event and the individual’s medical history are critical in determining the likelihood of Epilepsy and the need for further investigation:
- First-time seizure: Anyone experiencing a seizure for the first time should seek immediate medical attention, typically in an emergency room setting. This allows for a thorough initial assessment to identify any immediate underlying causes (such as head injury, fever, or metabolic disturbances) and to evaluate the risk of future seizures.
- Recurrent seizures: Individuals who have experienced more than one unprovoked seizure (a seizure not directly triggered by an acute illness or injury) should consult a neurologist, preferably one specializing in Epilepsy, for a comprehensive evaluation and potential diagnosis of Epilepsy.
- Changes in seizure pattern or frequency: For individuals already diagnosed with Epilepsy, any significant change in the frequency, type, or severity of their seizures warrants a prompt medical review.
Seeking timely medical advice is crucial for several reasons. Firstly, it allows for accurate diagnosis and differentiation of Epilepsy from other conditions that may mimic seizures. Secondly, it enables the initiation of appropriate treatment strategies aimed at controlling seizures and preventing future episodes.
Causes of Epilepsy
The underlying causes of Epilepsy are diverse and can vary depending on the individual’s age, medical history, and other factors. In a significant proportion of cases, particularly in childhood-onset Epilepsy, no specific cause can be identified, and it is classified as idiopathic Epilepsy, believed to have a strong genetic basis. However, when a cause can be determined, it often falls into one of several categories: Read More>>>>
Biological Causes
- Genetic Factors: Epilepsy has a well-established genetic component. Many different genes have been linked to an increased risk of developing Epilepsy or specific epilepsy syndromes. These genes can affect various aspects of brain function, including neuronal excitability and synaptic transmission.
- Structural Brain Abnormalities: Damage or malformations in the brain’s structure can disrupt normal electrical activity and lead to seizures. These abnormalities can arise from various causes, including:
- Stroke: Disruption of blood flow to the brain can cause brain damage and subsequent Epilepsy, particularly in older adults.
- Traumatic Brain Injury (TBI): Significant head injuries can scar brain tissue, increasing the risk of post-traumatic Epilepsy, which can develop months or even years after the injury.
- Brain Tumors or Cysts: Abnormal growths in the brain can compress or invade brain tissue, leading to seizures.
- Congenital Malformations: Abnormalities in brain development that occur before birth can predispose individuals to Epilepsy.
- Vascular Malformations: Abnormal formations of blood vessels in the brain can also cause seizures.
- Infections of the Brain: Infections such as meningitis (inflammation of the membranes surrounding the brain and spinal cord) and encephalitis (inflammation of the brain itself) can cause temporary or permanent brain damage that may lead to Epilepsy.
- Neurodegenerative Diseases: Conditions like Alzheimer’s disease and other forms of dementia can be associated with an increased risk of late-onset Epilepsy.
Lifestyle Triggers
While not the root cause of Epilepsy, certain lifestyle factors can lower the seizure threshold and trigger seizures in individuals with the condition:
- Sleep Deprivation: Insufficient or disrupted sleep is a common seizure trigger for many people with Epilepsy. Maintaining a regular and adequate sleep schedule is crucial for seizure management.
- Stress: Both physical and emotional stress can increase the likelihood of seizures in some individuals. Developing effective stress management techniques can be beneficial.
- Hormonal Changes: Fluctuations in hormone levels, particularly in women during their menstrual cycle (catamenial Epilepsy), can trigger seizures.
- Alcohol Consumption and Withdrawal: Excessive alcohol intake or abrupt withdrawal can lower the seizure threshold and precipitate seizures.
Identifying and, where possible, avoiding personal seizure triggers can be an important component of Epilepsy management, alongside medical treatments.
Risk Factors
Several factors can increase an individual’s susceptibility to developing Epilepsy:
- Family History of Epilepsy: Having a close relative with Epilepsy increases the risk, suggesting a genetic predisposition.
- Head Trauma: As mentioned earlier, significant head injuries are a known risk factor for post-traumatic Epilepsy.
- Stroke and Other Cerebrovascular Diseases: Conditions that affect blood flow to the brain can increase the risk of seizures.
- Brain Tumors or Lesions: Abnormal growths or damage in the brain can disrupt electrical activity.
- Infections of the Brain or Spinal Cord: Past infections can leave residual brain damage that may lead to Epilepsy.
- Developmental Disorders: Individuals with neurodevelopmental conditions like autism spectrum disorder and cerebral palsy have a higher incidence of Epilepsy.
- Premature Birth and Low Birth Weight: These factors can be associated with increased neurological vulnerabilities.
- Alzheimer’s Disease and Other Dementias: These neurodegenerative conditions increase the risk of late-onset seizures.
Understanding these risk factors can help identify individuals who may benefit from increased awareness and potentially earlier intervention if symptoms arise.

Complications
Uncontrolled or poorly managed Epilepsy can lead to a range of significant complications that impact physical safety, cognitive function, psychological well-being, and overall quality of life:
- Physical Injuries: Seizures can cause falls, leading to fractures, head injuries, and other trauma.
- Drowning: Seizures occurring during swimming or bathing pose a serious risk of drowning.
- Status Epilepticus: This is a life-threatening condition characterized by a prolonged seizure lasting more than five minutes or recurrent seizures without regaining consciousness between them. It requires immediate medical treatment to prevent permanent brain damage or death.
- Sudden Unexpected Death in Epilepsy (SUDEP): This is a rare but devastating complication where a person with Epilepsy dies suddenly without an apparent cause. The exact mechanisms of SUDEP are not fully understood, but uncontrolled seizures are a significant risk factor.
- Cognitive Impairment: Chronic seizures and some anti-seizure medications can contribute to difficulties with memory, attention, and learning.
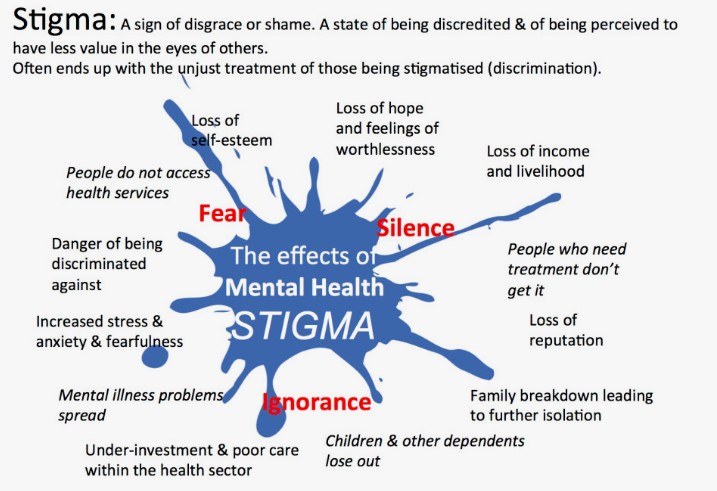
- Psychological Issues: Individuals with Epilepsy are at an increased risk of developing anxiety, depression, and social isolation due to the unpredictable nature of seizures and the associated stigma.
- Social and Occupational Limitations: The fear of seizures can limit participation in social activities, sports, and employment opportunities, impacting self-esteem and overall quality of life.
Effective management of Epilepsy, primarily through medication and lifestyle adjustments, aims to minimize the frequency and severity of seizures, thereby reducing the risk of these potentially serious complications.
Diagnosis
A thorough and accurate diagnosis is the cornerstone of effective Epilepsy management. It typically involves a combination of the individual’s medical history, a detailed description of seizure events, and several diagnostic tests:
- Electroencephalogram (EEG): This non-invasive test is the primary diagnostic tool for Epilepsy. Electrodes are attached to the scalp to record the electrical activity of the brain. Abnormal patterns of brain waves, such as spikes or sharp waves, can indicate a predisposition to seizures or the presence of interictal (between seizures) epileptiform discharges.
- Magnetic Resonance Imaging (MRI): An MRI scan of the brain provides detailed images of the brain’s structure. It is crucial for identifying any structural abnormalities that may be the underlying cause of seizures, such as tumors, lesions, vascular malformations, or hippocampal sclerosis (scarring in the temporal lobe, a common cause of focal seizures).
- Blood Tests: Routine blood tests are often performed to rule out other medical conditions that could be contributing to seizures, such as infections, electrolyte imbalances, or metabolic disorders.
In addition to these primary tests, the diagnostic process may also involve:
- Detailed Medical History: The neurologist will ask comprehensive questions about the individual’s seizure history, including the frequency, duration, and characteristics of the seizures, as well as any potential triggers. Past medical history, family history of seizures, and medication history are also important.
- Neurological Examination: A physical and neurological examination is conducted to assess the individual’s overall neurological function, including reflexes, coordination, and mental status.
- Video-EEG Monitoring: In some cases, prolonged monitoring with simultaneous video and EEG recording may be necessary to capture seizure events and correlate the clinical manifestations with the electrical activity in the brain.
The information gathered from these various sources is carefully integrated by the neurologist to arrive at an accurate diagnosis of Epilepsy, classify the type of seizures, and determine the most appropriate treatment plan.
Treatment Options
The primary goal of Epilepsy treatment is to achieve seizure freedom with minimal side effects, thereby improving the individual’s quality of life. A multifaceted approach is often employed, involving medication, lifestyle adjustments, and in some cases, more specialized interventions:
- Anti-Seizure Medications (ASMs): These are the cornerstone of Epilepsy treatment for most individuals. There are many different types of ASMs available, and the choice of medication depends on the type of seizures, the individual’s age, other medical conditions, and potential side effects.
- Vagus Nerve Stimulation (VNS): This is a neuromodulation therapy used for individuals with focal seizures that are not well-controlled by medication. A small device is surgically implanted under the skin in the chest, and a wire is threaded to the vagus nerve in the neck.
- Lifestyle Adjustments: Alongside medical treatment, lifestyle modifications play a crucial role in managing Epilepsy:
- Adequate Sleep: Maintaining a regular and sufficient sleep schedule is essential to avoid sleep deprivation, a common seizure trigger.
- Stress Management: Developing healthy coping mechanisms for stress can help reduce seizure susceptibility.
- Avoiding Known Triggers: Identifying and minimizing exposure to personal seizure triggers, such as flashing lights or alcohol, is important.
- Healthy Diet and Exercise: Maintaining a balanced diet and engaging in regular physical activity can contribute to overall well-being and potentially improve seizure control. You might find helpful information on /natural-remedies-for-epilepsy.
- Surgery: For individuals whose seizures originate from a specific, identifiable area of the brain that can be safely removed without causing significant neurological deficits, surgery may be a viable option to reduce or even eliminate seizures.
The management of Epilepsy is often a long-term process that requires ongoing collaboration between the individual, their family, and a team of healthcare professionals, including neurologists, nurses, and other specialists. Regular follow-up appointments are essential to monitor seizure control, adjust medications as needed, and address any concerns or side effects.