Discover the symptoms, root causes, and science-backed treatments for Diabetes (Type 2). Learn when to seek help and how to manage it effectively.
Overview
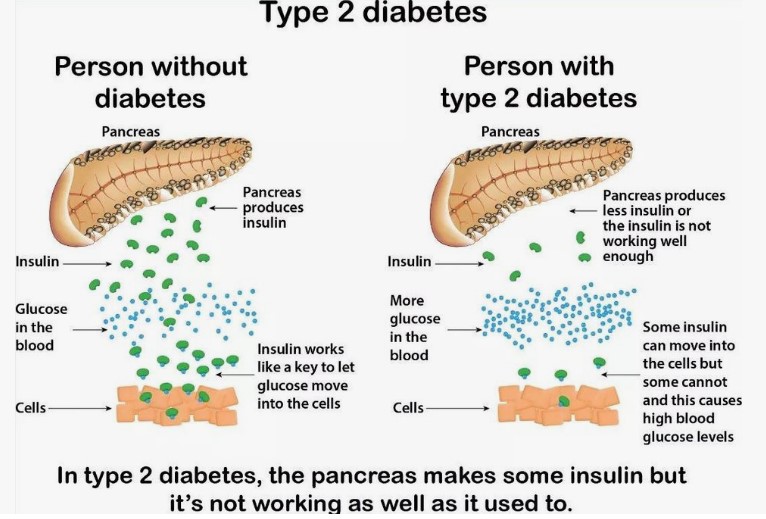
Have you ever noticed an unquenchable thirst that water alone cannot satisfy, or a persistent fatigue that lingers despite adequate rest? These subtle shifts in your body’s signals could be early whispers of a condition affecting a significant portion of the global adult population: Diabetes (Type 2). This intricate metabolic disorder is characterized by a sustained elevation of blood glucose levels, a consequence of either the body’s insufficient production of insulin or its cells’ diminished responsiveness to this crucial hormone. Insulin, a vital messenger synthesized by the pancreas, plays the pivotal role of escorting glucose, derived from the food we consume, into our cells where it is metabolized for energy. In the context of Diabetes (Type 2), this process becomes disrupted, leading to a buildup of glucose in the bloodstream, a state that, over time, can have far-reaching implications for overall health and well-being.
The prevalence of Diabetes (Type 2) has witnessed a dramatic surge in recent decades, reflecting evolving dietary habits, increasingly sedentary lifestyles, and a complex interplay of genetic predispositions. While precise, universally agreed-upon recent global statistics can fluctuate depending on the source and reporting period, it is unequivocally recognized by major health organizations worldwide that the incidence of this condition is a significant and growing public health concern. Understanding the nuances of Diabetes (Type 2), from its subtle initial manifestations to its potential long-term consequences, is paramount for fostering early detection, implementing effective management strategies, and ultimately empowering individuals to lead healthier lives despite this diagnosis. This article aims to delve into the multifaceted aspects of Diabetes (Type 2), exploring its characteristic symptoms, underlying causes, associated risk factors, potential complications, diagnostic pathways, and a spectrum of proven solutions for effective management.
Symptoms of Diabetes (Type 2)
The onset of Diabetes (Type 2) can often be insidious, with symptoms developing gradually over time, sometimes so subtly that they may go unnoticed for years. Recognizing these early warning signs is crucial for timely diagnosis and intervention. While the constellation of symptoms can vary among individuals, several key indicators frequently manifest:
- Increased thirst (polydipsia): This persistent and often excessive feeling of thirst arises as the body attempts to dilute the high concentration of glucose in the bloodstream. Despite increased fluid intake, the thirst may remain unquenched.
- Frequent urination (polyuria): Elevated blood glucose levels overwhelm the kidneys’ capacity to reabsorb glucose back into the bloodstream. As a result, the body tries to eliminate the excess glucose through urine, leading to increased frequency of urination, particularly at night.
- Increased hunger (polyphagia): Despite elevated blood glucose levels, the body’s cells are not receiving adequate energy due to insulin resistance. This cellular starvation can trigger persistent feelings of hunger, even after eating.
- Unexplained weight loss: Paradoxically, despite increased hunger and food intake, some individuals with undiagnosed Diabetes (Type 2) may experience unintentional weight loss. This occurs because the body is unable to utilize glucose for energy effectively and may start breaking down muscle and fat for fuel.
- Blurred vision: High blood glucose levels can affect the lens of the eye, causing it to swell and change shape, leading to temporary blurred vision. This symptom may fluctuate as blood glucose levels vary.
Beyond these primary symptoms, individuals with Diabetes (Type 2) may also experience:
- Fatigue and lethargy: The body’s inability to efficiently utilize glucose for energy can result in persistent feelings of tiredness and lack of energy.
- Slow-healing sores or frequent infections: High blood glucose levels can impair the body’s immune function and ability to heal, leading to slow-healing cuts, bruises, and more frequent infections, particularly of the skin, urinary tract, and gums.
- Numbness or tingling in the hands and feet (paresthesia): Over time, high blood glucose can damage nerves, leading to sensations of numbness, tingling, or pain, particularly in the extremities.
- Darkening of skin in the folds of the neck, armpits, or groin (acanthosis nigricans): This skin condition can be a sign of insulin resistance, a key underlying factor in Diabetes (Type 2).
It is important to note that not everyone with Diabetes (Type 2) will experience all of these symptoms, and some individuals may have very mild or no noticeable symptoms in the early stages. This underscores the importance of awareness, especially for those with known risk factors.
When to See a Doctor
Prompt medical attention is crucial if you experience any of the persistent or concerning symptoms associated with Diabetes (Type 2), particularly the classic triad of increased thirst, frequent urination, and unexplained weight loss. Ignoring these early warning signs can delay diagnosis and allow the condition to progress, potentially increasing the risk of long-term complications.
Furthermore, individuals with identified risk factors for Diabetes (Type 2) should engage in regular health screenings and discuss their risk with their healthcare provider. These risk factors include:
- Family history of diabetes: Having a parent, sibling, or close relative with Diabetes (Type 2) significantly increases your risk.
- Being overweight or obese: Excess body weight, particularly abdominal fat, is strongly linked to insulin resistance.
- Older age: The risk of developing Diabetes (Type 2) increases with age, particularly after the age of 45.
- History of gestational diabetes: Women who developed diabetes during pregnancy (gestational diabetes) have a higher risk of developing Diabetes (Type 2) later in life.
- Physical inactivity: A sedentary lifestyle contributes to insulin resistance and increases the risk of weight gain.
- High blood pressure (hypertension): Hypertension often coexists with insulin resistance and increases the risk of cardiovascular complications.
- Abnormal cholesterol levels: High levels of LDL (“bad”) cholesterol and low levels of HDL (“good”) cholesterol are associated with an increased risk of Diabetes (Type 2).
- Certain ethnicities: Individuals of certain racial and ethnic backgrounds, including African Americans, Hispanic/Latino Americans, American Indians, Pacific Islanders, and Asian Americans, have a higher prevalence of Diabetes (Type 2).
Regular check-ups, even in the absence of obvious symptoms, are particularly important for individuals with these risk factors. Healthcare providers can assess individual risk, recommend appropriate screening tests, and provide guidance on lifestyle modifications to help prevent or delay the onset of Diabetes (Type 2). Early diagnosis allows for timely intervention, which can significantly improve long-term health outcomes and reduce the risk of complications.

Causes of Diabetes (Type 2)
The development of Diabetes (Type 2) is a complex process involving a confluence of genetic predispositions, metabolic dysfunctions, and environmental factors, particularly lifestyle choices. Understanding these intricate causes is essential for developing effective prevention and management strategies. The primary underlying mechanisms driving Diabetes (Type 2) can be broadly categorized into biological causes and lifestyle triggers. Also Read>>>>>
Biological Causes
The cornerstone of Diabetes (Type 2) pathogenesis lies in two interconnected biological processes:
- Insulin Resistance: This is the primary defect in most individuals with Type 2 diabetes. Insulin, a hormone produced by the beta cells of the pancreas, acts as a key that unlocks the doors of cells, allowing glucose from the bloodstream to enter and be used for energy. In insulin resistance, these cellular doors become less responsive to insulin’s signal, requiring the pancreas to produce more and more insulin to try and overcome this resistance and maintain normal blood glucose levels. Over time, the pancreas may become overworked and eventually lose its capacity to produce sufficient insulin to meet the body’s needs. The exact molecular mechanisms underlying insulin resistance are multifaceted and involve complex interactions between genetic factors, cellular signaling pathways, and the influence of excess body fat, particularly visceral fat (fat stored around the abdominal organs).
- Impaired Insulin Secretion: While insulin resistance is often the initial trigger, many individuals with Diabetes (Type 2) also experience a progressive decline in the ability of their pancreatic beta cells to secrete adequate amounts of insulin. This impairment can be due to a variety of factors, including the chronic stress placed on the beta cells by prolonged insulin resistance, genetic predispositions affecting beta cell function, and the toxic effects of chronically elevated blood glucose levels (glucotoxicity) and elevated free fatty acids (lipotoxicity) on these cells. As the beta cells lose their functional capacity, they are unable to produce enough insulin to compensate for the existing insulin resistance, leading to a further rise in blood glucose levels and the eventual manifestation of Diabetes (Type 2).
The interplay between genetic susceptibility and these metabolic disturbances is significant. Certain genes can increase an individual’s predisposition to both insulin resistance and impaired insulin secretion. While a specific “diabetes gene” has not been identified, multiple genes are thought to contribute to the overall risk. These genes may influence factors such as beta cell development and function, insulin signaling pathways, and the regulation of glucose metabolism.
Lifestyle Triggers
While biological factors create a foundation of susceptibility, lifestyle choices play a pivotal role in triggering and accelerating the development of Diabetes (Type 2). Several key lifestyle factors have been consistently linked to an increased risk:
- Obesity and Overweight: Excess body weight, particularly the accumulation of visceral fat, is a major driver of insulin resistance. Adipose tissue (fat tissue) releases various hormones and inflammatory molecules that can interfere with insulin signaling and reduce insulin sensitivity in cells. The increased metabolic demand in individuals with obesity also puts a greater strain on the pancreas to produce sufficient insulin.
- Physical Inactivity: Regular physical activity enhances insulin sensitivity, meaning that the body’s cells become more responsive to insulin, allowing glucose to be taken up more efficiently from the bloodstream. Conversely, a sedentary lifestyle contributes to insulin resistance and increases the risk of weight gain, further exacerbating the problem. Muscle contraction during exercise also has an insulin-independent effect on glucose uptake by muscle cells.
- Unhealthy Diet: Diets high in processed foods, sugary drinks, saturated and trans fats, and low in fiber can contribute to weight gain, insulin resistance, and impaired glucose metabolism. The rapid absorption of sugars from refined carbohydrates and sugary beverages leads to sharp spikes in blood glucose levels, placing a greater burden on the pancreas. Chronic consumption of unhealthy fats can also contribute to inflammation and insulin resistance.
- Chronic Stress: Prolonged stress can trigger the release of stress hormones, such as cortisol and adrenaline, which can raise blood glucose levels and contribute to insulin resistance over time. Stress can also indirectly influence dietary choices and physical activity levels, further increasing the risk of Diabetes (Type 2).
- Sleep Deprivation: Emerging research suggests a link between inadequate sleep and an increased risk of insulin resistance and impaired glucose tolerance. Sleep deprivation can disrupt hormonal balance, including hormones that regulate appetite and glucose metabolism.
The interaction between these biological predispositions and lifestyle triggers is crucial in the development of Diabetes (Type 2). Individuals with a genetic susceptibility may be more vulnerable to the negative effects of unhealthy lifestyle choices, leading to an earlier onset or more severe form of the disease. Conversely, adopting a healthy lifestyle can significantly mitigate the risk even in individuals with a strong family history of diabetes.
Risk Factors
As previously mentioned, numerous factors can elevate an individual’s likelihood of developing Diabetes (Type 2). Identifying these risk factors is essential for targeted prevention efforts and early screening. A comprehensive understanding of these factors allows both individuals and healthcare professionals to proactively manage risk and potentially delay or prevent the onset of the disease. The key risk factors include:
- Family History: A strong family history of Diabetes (Type 2), particularly in first-degree relatives (parents, siblings), significantly increases an individual’s risk. This highlights the role of genetic factors in susceptibility to the disease.
- Obesity and Overweight: Excess body weight, defined by a Body Mass Index (BMI) of 25 or higher for overweight and 30 or higher for obesity, is a major modifiable risk factor. The accumulation of excess fat tissue, especially visceral fat, contributes significantly to insulin resistance.
- Age: The risk of developing Diabetes (Type 2) increases with age, particularly after the age of 45. This may be due to age-related declines in beta cell function and increased insulin resistance.
- Gestational Diabetes: Women who develop gestational diabetes during pregnancy have a substantially higher risk (up to 50%) of developing Diabetes (Type 2) later in life. Gestational diabetes indicates a predisposition to impaired glucose tolerance.
- Physical Inactivity: A sedentary lifestyle is a significant independent risk factor for Diabetes (Type 2). Regular physical activity improves insulin sensitivity, helps with weight management, and has beneficial effects on glucose metabolism.
- High Blood Pressure (Hypertension): Hypertension often clusters with insulin resistance, obesity, and dyslipidemia (abnormal cholesterol levels), increasing the overall risk of cardiovascular disease and Diabetes (Type 2).
- Abnormal Cholesterol Levels (Dyslipidemia): High levels of LDL (“bad”) cholesterol and triglycerides, and low levels of HDL (“good”) cholesterol, are associated with an increased risk of insulin resistance and Diabetes (Type 2).
- Prediabetes: Individuals with prediabetes, a condition characterized by blood glucose levels higher than normal but not yet in the diabetic range, are at high risk of progressing to Diabetes (Type 2). Identifying and managing prediabetes through lifestyle changes can often prevent or delay this progression.
- Certain Ethnicities: As noted earlier, certain racial and ethnic groups have a higher prevalence of Diabetes (Type 2), suggesting a potential interplay of genetic and environmental factors within these populations.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS, a hormonal disorder, often experience insulin resistance and have an increased risk of developing Diabetes (Type 2).
- History of Cardiovascular Disease: Individuals with a history of heart disease or stroke are at an increased risk of developing Diabetes (Type 2), and vice versa, highlighting the interconnectedness of these conditions.
Recognizing these risk factors empowers individuals to take proactive steps to mitigate their risk through lifestyle modifications and regular medical check-ups. Healthcare providers can use this information to identify high-risk individuals and implement targeted prevention strategies.
Complications
The chronic hyperglycemia (high blood glucose levels) characteristic of poorly managed Diabetes (Type 2) can lead to a wide array of serious long-term complications affecting various organ systems. These complications develop over time due to damage to blood vessels and nerves caused by sustained high glucose levels. Effective management of blood glucose, blood pressure, and cholesterol levels is crucial to prevent or delay the onset and progression of these debilitating complications. The major long-term complications of Diabetes (Type 2) include:
- Cardiovascular Disease: Diabetes significantly increases the risk of developing various forms of cardiovascular disease, including coronary artery disease (leading to angina and heart attacks), stroke, peripheral artery disease (PAD), and heart failure. High blood glucose levels can damage blood vessels, promoting atherosclerosis (hardening and narrowing of the arteries), which restricts blood flow and increases the risk of these events.
- Neuropathy (Nerve Damage): High blood glucose can damage nerves throughout the body, leading to various forms of neuropathy. Peripheral neuropathy, affecting the nerves in the hands and feet, is the most common type, causing symptoms such as numbness, tingling, pain, and loss of sensation. Autonomic neuropathy can affect nerves controlling involuntary functions such as digestion, heart rate, blood pressure, and bladder function.
- Nephropathy (Kidney Damage): The kidneys filter waste products from the blood. In diabetes, high blood glucose can damage the small blood vessels in the kidneys, impairing their filtering ability. Over time, this can lead to chronic kidney disease and eventually kidney failure, requiring dialysis or kidney transplantation.
- Retinopathy (Eye Damage): Diabetes is a leading cause of blindness. High blood glucose can damage the small blood vessels in the retina, the light-sensitive tissue at the back of the eye. This can lead to various eye problems, including diabetic retinopathy (damage to blood vessels), macular edema (swelling in the central part of the retina), cataracts (clouding of the lens), and glaucoma (increased pressure inside the eye), all of which can impair vision and eventually cause blindness if left untreated.
- Foot Problems: Nerve damage (neuropathy) and poor blood circulation (due to blood vessel damage) in the feet can lead to serious foot problems in people with diabetes. Even minor cuts or blisters can become infected and heal poorly, potentially leading to ulcers, gangrene, and the need for amputation.
- Skin Problems: People with diabetes are more prone to various skin conditions, including bacterial and fungal infections, itching, and dry skin. Acanthosis nigricans, a darkening of skin folds, can also occur.
- Hearing Impairment: Studies have shown a link between diabetes and an increased risk of hearing loss, although the exact mechanisms are not fully understood.
- Alzheimer’s Disease and Cognitive Decline: Emerging research suggests a possible link between diabetes and an increased risk of Alzheimer’s disease and other forms of cognitive decline, although more research is needed to fully understand this association.
- Increased Risk of Infections: High blood glucose can weaken the immune system, making individuals with diabetes more susceptible to various infections, including urinary tract infections, pneumonia, and flu.
The development and severity of these complications are directly related to the duration and control of blood glucose levels. Maintaining near-normal blood glucose levels through effective management strategies significantly reduces the risk of these long-term consequences, emphasizing the importance of early diagnosis, comprehensive treatment, and ongoing self-management education.
Diagnosis
The diagnosis of Diabetes (Type 2) typically involves several blood tests that measure blood glucose levels at different times and under different conditions. These tests help determine if an individual’s blood glucose levels are consistently elevated above the normal range. The primary diagnostic tests for Diabetes (Type 2) include:
- Fasting Plasma Glucose (FPG) Test: This test measures blood glucose levels after an overnight fast of at least 8 hours. A fasting plasma glucose level of 126 milligrams per deciliter (mg/dL) or higher on two separate occasions indicates diabetes. A level between 100 and 125 mg/dL is considered prediabetes.
- Hemoglobin A1c (HbA1c) Test: This test provides an average of blood glucose levels over the past 2-3 months. It measures the percentage of hemoglobin (a protein in red blood cells that carries oxygen) that has glucose attached to it. The higher the blood glucose levels have been over time, the more glucose will be attached to hemoglobin. An A1c level of 6.5% or higher indicates diabetes. A level between 5.7% and 6.4% is considered prediabetes. This test does not require fasting and provides a longer-term picture of blood glucose control.
- Random Plasma Glucose Test: This test measures blood glucose levels at any time of day, without regard to the last meal. A random plasma glucose level of 200 mg/dL or higher, along with symptoms of diabetes (such as increased thirst, frequent urination, and unexplained weight loss), can suggest diabetes. However, a positive random glucose test usually needs to be confirmed with a fasting plasma glucose test or
Sources and related content